

People with diabetes know that carb-counting is important. That’s because carbohydrates (carbs) have a big impact on your blood sugar. But does it matter what carbs you’re counting? Absolutely. Not all carbs are equal. While you want to keep an eye on your total carb intake, it’s important to remember that some carbs are better for your overall health.
Carbs can be one of three things: sugars, starches, or fibers. Sugar can be found naturally, for example in milk and fruit, but it’s the added sugar you really want to avoid. Added sugar is what you’ll find in a cookie for example, but it’s often snuck into processed foods to preserve them and make them taste better. So it’s wise to steer clear of processed foods. Try to get most of your carbs from fiber and load up on the healthy carbs found in high-fiber foods like whole grain products and vegetables.

Losing weight can help you manage type 2 diabetes. But doing so can be frustrating. Many people who lose weight try for a few weeks or a month, get discouraged, and resume their old habits. Here are some tips for a weight loss regimen you can stick with:

Americans get less sleep than they used to, and the sleep they do get is more fragmented. That’s bad news for people with diabetes. Not getting 6.5 to 8.5 hours of sleep has been shown to increase your blood glucose level.
There’s a little bit of a catch, though. If you’re one of those people who gets more than 8.5 hours of sleep, you could be at greater risk, too. So getting just the right amount of sleep is key. To regulate your sleep patterns, try these tips:

People with diabetes need to be especially vigilant when it comes to getting physical throughout the day. If you’re like most Americans, you probably spend long periods of time without moving around much, but that can make it tough to manage your blood sugar.
Instead, the American Diabetes Association recommends a little physical activity every 30 minutes for people who sit throughout the day. That means office workers with diabetes should take special care to get a few minutes of activity in throughout their workday. When you’re sedentary, especially when watching TV, your diabetes and obesity risks rise. How can you stay active every half hour? First off, the ADA distinguishes “physical activity†from “exercise.†You don’t need a full-blown workout to get a little more active throughout the day. Here are some tips:

If you have diabetes, you should be familiar with regular blood testing. This is the most important tool in your arsenal for monitoring your blood sugar levels. Individual target ranges for blood glucose vary, but the American Diabetes Association has released recommendations for adults who are not pregnant: Aim for an A1C of 7% (eAG 154 mg/dl). Prior to a meal, aim for 80-130 mg/dl, and less than 180 mg/dl 1-2 hours after the start of a meal.
Who Should Test Daily?
New recommendations state that all adults over age 18 with type 1 diabetes should test daily. (Older recommendations suggested starting at age 25). Self-monitoring for type 2 diabetes also has benefits, but the benefits aren’t nearly so clear if you don’t take insulin. In that case you should check with your doctor.
Another new recommendation from the ADA involves people with high blood pressure (hypertension). If you have this and diabetes, you’ll need to do more than just monitor at home. Monitor your blood sugar levels at the office as well as at home, which may give you needed information about how you can improve the way you take your medication.

People in the modern world face stress from various sources. It can be caused by a big test, a demanding boss, or a traffic jam, among many other sources. Even if your stress is long-term, it primes your body for an immediate reaction—this is the so-called fight-or-flight response. That may be great in nature when you need to escape from a wild beast, but it doesn’t work as well if your source of stress is caring for an aging parent. In addition to other health problems, stress can change your blood glucose.
The relationship between stress and diabetes is complicated. People with type 2 diabetes see their blood sugar levels shoot up while stressed. People with type 1 diabetes may see their blood sugar rise under stress, or they may see it dip. Physical stress raises your blood sugar levels higher than mental stress no matter what type of diabetes you have.
Coping With Stress
For your continued health, you need to get good at dealing with stress—especially if you have diabetes. Fortunately there are many relaxing ways to accomplish this:

People with type 2 diabetes are at a high risk of developing heart disease, a condition responsible for 1 in 4 deaths in the U.S. each year. Consuming too much sodium leaves you at even greater risk, because sodium can increase your blood pressure and also dampen the effectiveness of blood pressure medicine.
Even so, you don’t want to get too little sodium in your diet either. Some diabetes experts warn that you risk additional health problems by eating too little salt. One study found that type 2 patients with the lowest sodium actually stood the highest risk of an early death.
The key to eating a healthy amount of sodium is to reduce your reliance on processed foods. Canned, frozen, and boxed foods tend to be too high in sodium, which is used as a preservative. So protect your heart by switching to fresh foods and keep your sodium levels in check. Also when cooking at home, choose spices that don’t have any added salt, and use these in place of your usual salt regimen.

The no. 1 cause of death and disease for diabetes patients is cardiovascular disease, also known as heart disease. One study found that more than 85% of diabetes patients also have high blood pressure, a precursor of heart disease. If you, like the majority of diabetes sufferers, have hypertension, it’s important that you check your blood pressure regularly at home. Here are some tips for doing this correctly:

The cell growth response to wounds is diminished for people with diabetes. This is one reason they are more prone to foot ulcers, a major cause of hospitalization for this population. The American Diabetes Association recommends treating cuts immediately with clean bandages. Major burns, cuts, and infections are serious enough for those with diabetes to require seeing a doctor right away. Scientists are working toward a cure for this serious health problem on various fronts, from tissue engineering research to studies on stem cells.

Everyone knows smoking is bad for your health. But that’s especially true for people with diabetes. Doctors have known for a long time that smokers with diabetes stand a greater risk of developing heart disease, kidney disease, poor circulation, vision problems, and nerve damage. Now they think they know why.
A chemistry professor studied human blood samples and found something surprising. Just adding nicotine to the blood samples sent the blood glucose level skyward. As it turns out, nicotine (found in nicotine gums and patches too, not just cigarettes) raises a person’s chances of developing diabetes by 30% to 40%. And if you already have diabetes, using nicotine makes it harder to control your symptoms.
Nicotine is notoriously addictive, and quitting can be tough. Your chances are better if you ask for help. Tell your doctor you want to get serious about quitting, and ask for suggestions and resources to support you in your journey to a healthier you.

When you live with diabetes, choosing a healthy meal takes on additional importance. There’s no such thing as a diabetes “superfood,†but there are better choices and worse choices. Foods that give you the best shot at controlling your diabetes symptoms are rich in nutrients like minerals, vitamins, and fiber but low on added sugar and starches.
The American Diabetes Association singles out a few solid choices for controlling your diabetes symptoms. While other foods are fine in the right proportions, these are some real winners you can’t go wrong with:

Getting sick is worse when you have diabetes. The flu brings the risk of more serious health complications like pneumonia, sinus infections, and bronchitis. Even more serious, sickness can raise your blood sugar, which can lead to the serious condition known as ketoacidosis for people with type 1 diabetes. Ketoacidosis symptoms include “fruity†smelling breath, vomiting, confusion and even unconsciousness. If you notice these signs, get emergency medical help immediately.
In general, you need to be more vigilant about monitoring your blood sugar while sick. You should check your blood sugar levels every four hours. Sometimes you lose your appetite when sick and this can be dangerous, too. If this happens to you, contact your health team. Vomiting is more serious for people with diabetes. If you are vomiting, go to the emergency room.
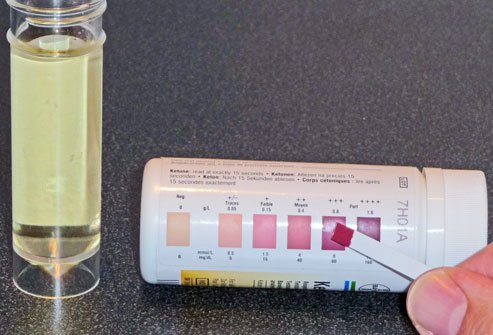
If you have type 1 diabetes, you need to keep ketone strips handy in case you get sick, and in case your blood sugar level stays higher than 240 for more than two hours. Also, pregnant women with type 1 diabetes should test their ketone levels every morning before eating.
Just keeping these strips handy isn’t enough, though. You need to make sure your ketone strips have not expired. Yes, these strips do expire. Depending on the manufacturer, your strips may expire anywhere from 6 months to a year from when you purchase them. Keep an eye on that expiration date and order more in advance of that date so you always have a ready supply.

School presents special challenges for children with diabetes. They probably don’t want to be singled out or to feel different, but the reality is that these kids do need special care. There are even laws set up to protect the rights of children to test their blood sugar levels and to treat low blood sugar when necessary—even during class. To minimize the sense of alienation diabetes can stir up, a child should be taught from an early age to self-manage his or her condition as much as possible. This is easier with the advice and support of a health care team trained to address a child’s needs and circumstances.

People with diabetes are vulnerable to diabetic eye disease, a catch-all term used for a variety of vision problems that include some of the most dangerous conditions. Cataracts and glaucoma risks increase with diabetes, and diabetic retinopathy is a particular danger. More people with diabetes experience vision loss from diabetic retinopathy—damaged blood vessels in the retina—than any other vision problem. Swelling of the eye lens and retina damage are other serious risks associated with diabetes.
Although these problems can be very serious, most of them can be controlled before they become major problems. Because people with diabetes have a greater risk of vision problems, special care needs to be taken to see your eye doctor regularly. You should have your retinas examined every two years—without testing, retinal damage can go unnoticed until it has done serious damage. Controlling your blood sugar helps reduce your risks as well.

When you’re traveling, diabetes requires special care. That’s especially true when you change time zones, which disrupts your body’s natural sleep/wake cycle and can throw off your body’s roduction of insulin and the timing of your medications. Travel can bring on stress and present you with unusual foods, and these can throw your body off as well.
You should pack with diabetes in mind. Bring a letter from your doctor that says you need access to diabetes medicine. Bring prescription labels and backup prescriptions, along with a list of any medications you take and how you take them. Don’t forget your blood sugar monitor, and bring extra batteries, lancets, and test strips in case you lose them or run out. Always travel with a quick carb snack. If you take insulin, know that time zone changes will require you to adjust your schedule. These calculations can be complicated, so have it figured out and written down before you leave.

People with diabetes are more likely to be dehydrated. When your blood sugar is too high, you may notice you get thirsty more easily. Listen to your thirst. Drinking water will not raise your blood glucose level, and it helps flush the excess glucose out of your system.
Drinking enough water may help you prevent diabetes in the first place. A decade-long study tracked more than 3,000 healthy people ages 30 to 65. It found that those who drank half a liter of more of water per day were about 30% less likely to develop hyperglycemia. The researchers cautioned that there could be other explanations for this group’s better odds of avoiding diabetes. It could be they are more active on average than those who drink less water, for example. Still, the research suggests staying hydrated might help you keep your blood sugar from skyrocketing.

Sometimes the warning signs of diabetes appear on your skin. People with diabetes are particularly prone to dry skin, which can be caused by high blood glucose. Dry skin also leaves you more vulnerable to infection. To prevent dry skin, avoid hot showers, spas, and bubble baths (they often have drying detergents). Try using moisturizing soaps and mild shampoos instead, and keep the shower water warm, but not too hot. When you get out of the tub, check your skin for red, sore, or dry areas that may be more prone to infection. Moisturizing after your bath or shower can help.
There are more potential skin problems for those with diabetes. Red, brown, or yellow skin patches that start as solid, raised bumps can develop. This is called necrobiosis lipoidica, and while harmless, can lead to more serious complications. Diabetes can also cause your skin to darken at creases under your armpits, at the groin, or on the back of your neck. This can be a sign your insulin is too high. Some people with especially difficult diabetes cases may develop hard, thick skin known as digital sclerosis. This skin condition mainly on the fingers and toes is described as giving your skin an orange peel texture and stiff joints.

One of the most important steps you can take to keep diabetes in control is to visit your doctor regularly. People with diabetes should plan to see their doctor two to four times a year. You may need more frequent medical visits if you take insulin, or if you are having difficulty balancing your blood sugar.
In addition to these doctor visits, schedule a yearly physical exam. You should make a yearly eye appointment as well. Make sure you’re screened for nerve, kidney, and eye issues. Visit your dentist twice a year. Whatever medical professional you meet, make sure he or she knows you have diabetes.
Reviewed by Charles Patrick Davis, MD, PhD on 2/7/2018
This tool does not provide medical advice. See additional information
© 1996-2018 WebMD, LLC. All rights reserved. Source slideshow at OnHealth